Are you ready to grow up your business? Contact Us
Call us anytime
Are you ready to grow up your business? Contact Us
CPT code 20611 is reported for ultrasound-guided arthrocentesis or injection of a major joint or bursa. To bill it correctly, physicians must document medical necessity, ultrasound guidance, permanent image recording, needle placement, joint treated, and modifier use when applicable. Missing any of these elements commonly leads to claim denials or audits.
CPT code 20611 describes ultrasound-guided arthrocentesis, aspiration, or injection of a major joint or bursa. The code includes real-time ultrasound visualization used to guide needle placement during the procedure.
Common joints reported under CPT 20611 include the knee, shoulder, hip, and other major joints. The ultrasound guidance is not optional. It is the defining element of the code.
This code is frequently used by orthopedists, rheumatologists, sports medicine physicians, pain specialists, and primary care providers.
CPT 20611 should be reported only when ultrasound guidance is medically necessary and actively used to guide the procedure.
Appropriate clinical indications include joint effusion, inflammatory arthritis, osteoarthritis flare, bursitis, or pain requiring therapeutic injection. The diagnosis must support why ultrasound guidance improves accuracy or safety.
If ultrasound is not used or documented, CPT 20611 should not be billed.
CPT 20611 documentation requirements are strict and closely reviewed by payers.
Your procedure note must clearly include:
Generic statements such as “ultrasound used” are insufficient. The documentation must show that the ultrasound directly guided the procedure, not merely assisted.
This level of detail protects against denials and post-payment audits.
Permanent recording and reporting are non-negotiable compliance requirements for CPT 20611.
Physicians must retain ultrasound images that demonstrate needle placement and joint visualization. These images must be stored in the patient’s medical record or imaging system.
The report should reference:
Failure to retain images is one of the most common reasons CPT 20611 claims are denied or recouped during audits.
Understanding CPT 20611 vs 20610 is critical for accurate coding.
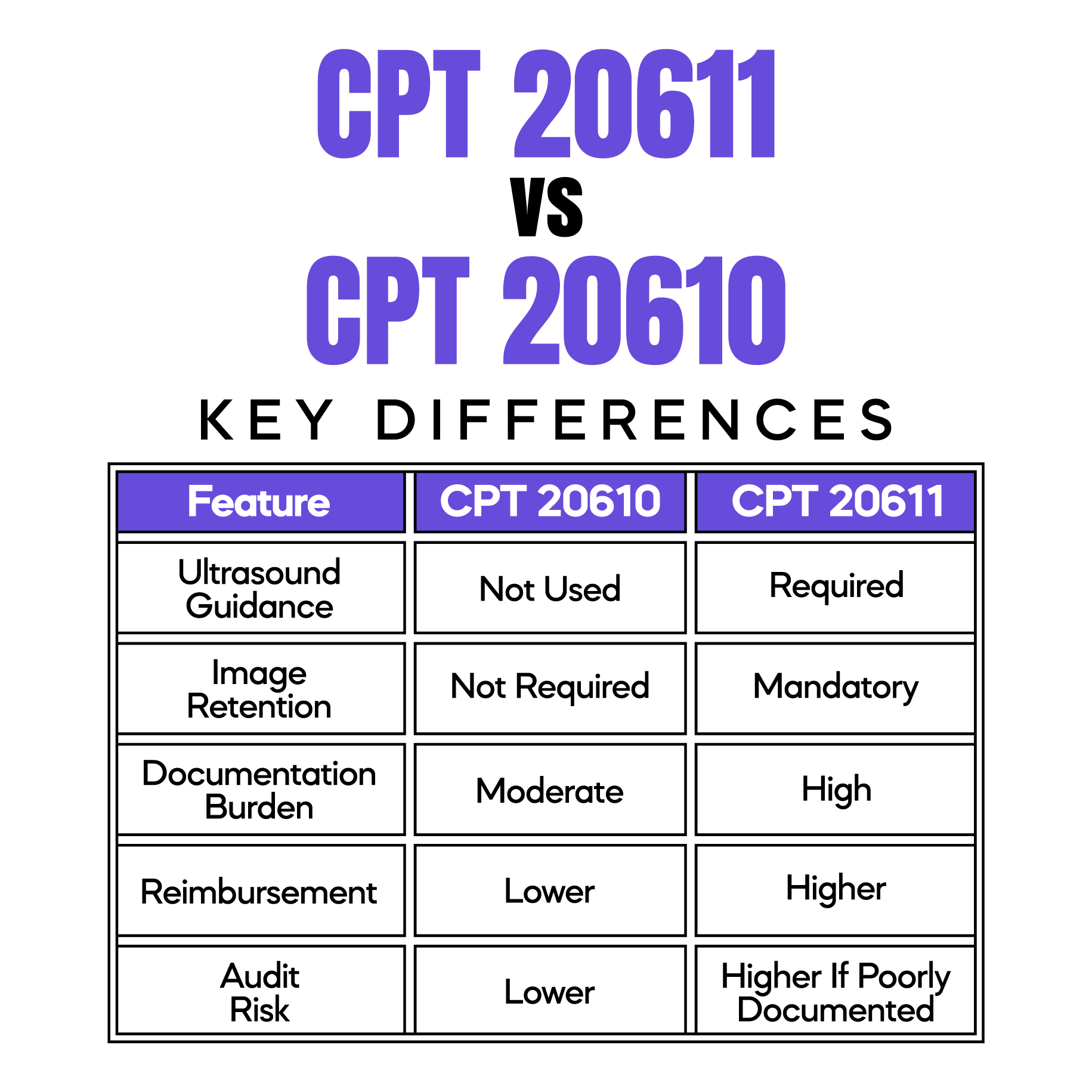
If ultrasound guidance is used but not documented properly, billing CPT 20611 increases audit exposure. In those cases, CPT 20610 may be more appropriate.
Modifier 50 for CPT 20611 is used when bilateral joints are treated during the same session.
However, payer rules vary. Some payers require:
Medicare typically allows modifier 50, but commercial payers may not. Incorrect modifier usage is a frequent denial trigger.
Always verify payer-specific bilateral reporting rules before claim submission.
The CPT 20611 reimbursement rate for 2026 varies by setting and geographic region.
In general:
Reimbursement accuracy depends heavily on documentation quality. Claims with missing ultrasound details or image retention references are often reduced or denied.
Ultrasound-guided arthrocentesis coding requires alignment between clinical care, documentation, and billing.
Best practices include:
These steps significantly reduce denial risk and improve payment timelines.
Understanding 20611 denial reasons helps prevent revenue loss.
The most common issues include:
Most denials are preventable with structured documentation and pre-submission review.
Arj Fatima is a senior medical billing and compliance specialist with extensive experience in U.S. procedural coding, physician documentation audits, and payer reimbursement policy. She focuses on helping physicians reduce denials, improve compliance, and protect revenue through accurate coding and education.
© Billing MedTech. All Rights Reserved