Are you ready to grow up your business? Contact Us
Call us anytime
Are you ready to grow up your business? Contact Us
High-cost skin biopsies play a critical role in dermatology, particularly when evaluating lesions with malignant potential. While these procedures are clinically justified in many cases, they remain one of the most frequently denied services in dermatology billing. The problem is rarely the biopsy itself. In most situations, denials occur because the documentation does not clearly demonstrate medical necessity from a payer’s perspective.
Dermatologists often assume that their clinical judgment is self-evident in the medical record. However, CMS and commercial payers require more than implied reasoning. They expect documentation that clearly explains why a biopsy was required, why it was performed at that visit, and why a specific biopsy technique was selected. When these elements are missing or vaguely documented, even appropriate biopsies can result in denied or downcoded claims.
High-cost biopsies are closely monitored because of their direct impact on payer spending and their potential for overutilization. CMS and insurers analyze biopsy patterns across dermatology practices to identify services that appear excessive or inconsistent with documented diagnoses. When a claim is reviewed, the payer is not evaluating clinical skill. They are evaluating whether the documentation supports that the service was reasonable and necessary for that specific patient.
For this reason, dermatology practices must view documentation as both a clinical record and a financial safeguard. Proper documentation reduces the likelihood of claim denials and protects the practice during audits.
Medical necessity in dermatology refers to the requirement for a biopsy to diagnose, confirm, or rule out a condition that cannot be safely or effectively managed through observation alone. The documentation must show that the lesion raised legitimate concern and that the biopsy outcome would influence patient management.
A simple statement such as “biopsy performed to rule out malignancy” is no longer sufficient. Payers expect to see clinical details that justify why malignancy was suspected and why tissue sampling was necessary at that point in care.
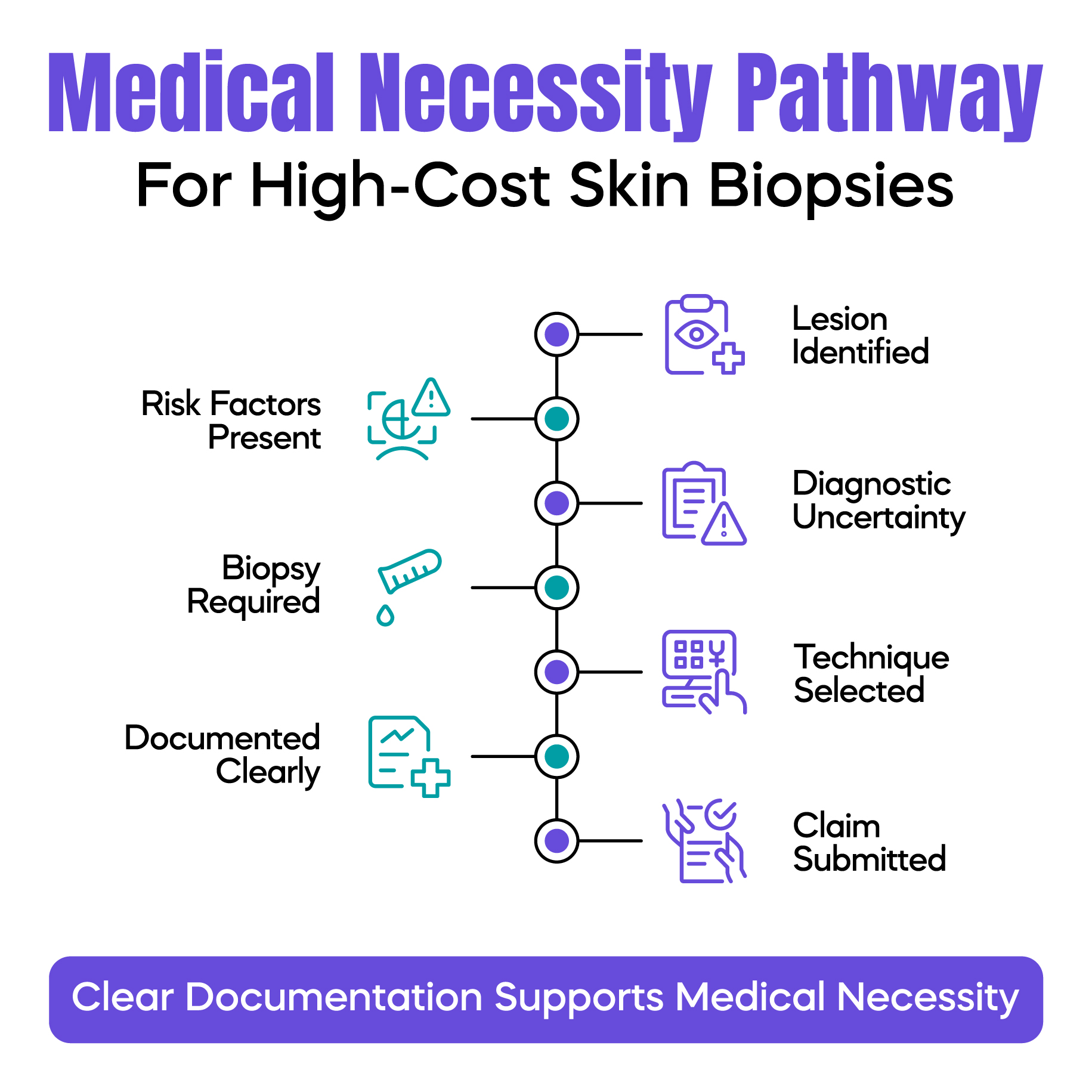
Every biopsy claim is reviewed with a set of implicit questions in mind. Payers want to know why the lesion was concerning, what clinical features supported that concern, and why the biopsy could not be delayed or avoided. They also assess whether the biopsy method chosen was appropriate for the lesion’s characteristics and location.
When documentation answers these questions clearly and logically, the claim becomes much easier to defend. When these questions are left unanswered, denials become far more likely.
Accurate lesion documentation forms the foundation of medical necessity. Vague descriptions such as “abnormal lesion” or “suspicious mole” do not provide enough clinical context for reviewers. Documentation should clearly describe the lesion’s location, size, appearance, and any notable changes reported by the patient or observed during examination.
Explaining features such as asymmetry, irregular borders, color variation, ulceration, bleeding, or rapid growth helps establish why observation was not appropriate. These details allow a reviewer to understand the level of risk that justified the biopsy.
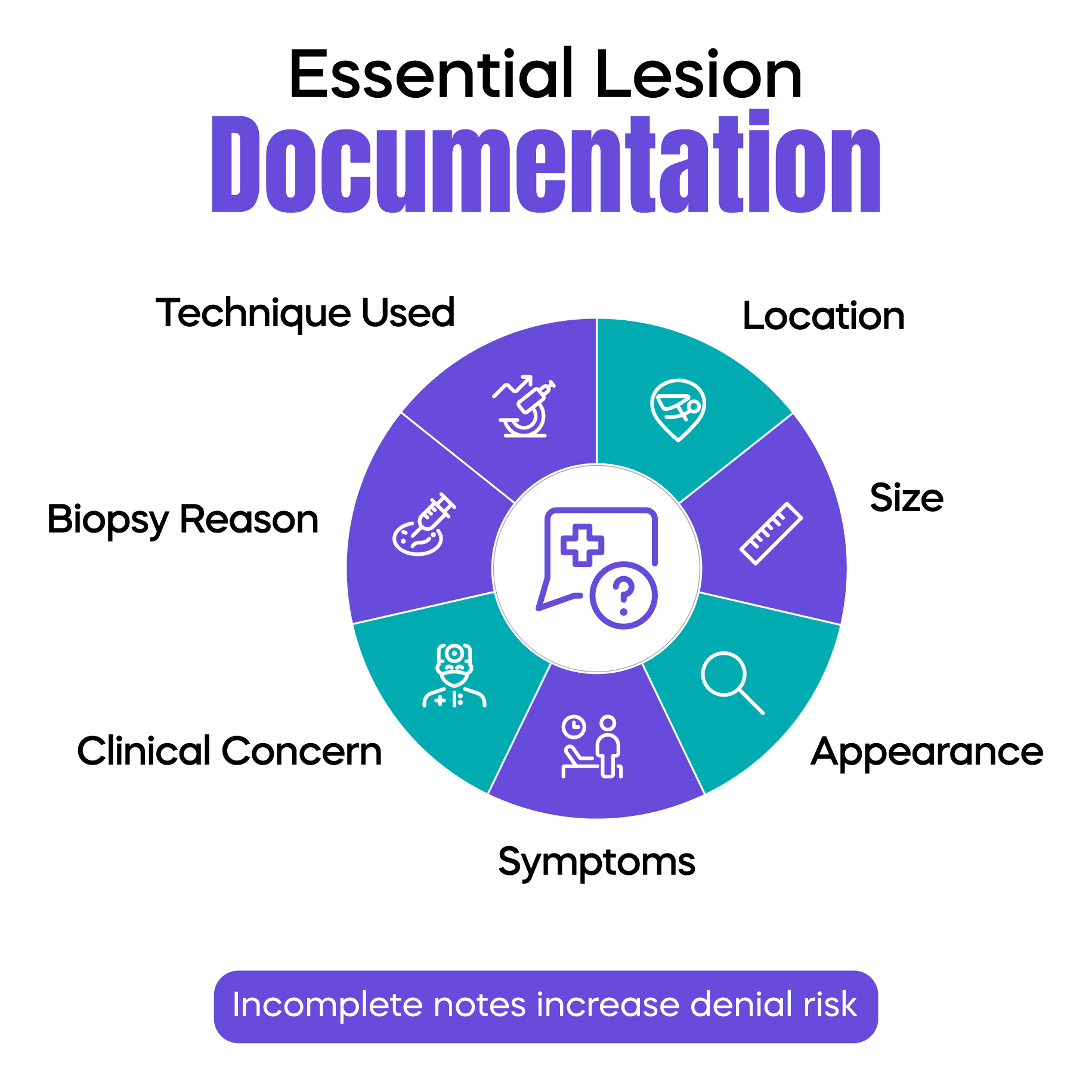
One of the most common documentation gaps occurs when clinical findings are recorded but not clearly linked to the biopsy decision. Simply listing lesion characteristics without explaining how they influenced clinical judgment weakens medical necessity.
Effective documentation explains the reasoning behind the decision. When clinical findings suggest possible malignancy or uncertain behavior, the record should clearly state that a biopsy was required to establish a diagnosis and guide further treatment. This narrative connection is essential for audit readiness.
High-cost biopsies require justification not only for why a biopsy was performed, but also for why a particular technique was selected. Whether a shave, punch, or excisional biopsy is used, the documentation should reflect why that method was clinically appropriate for the lesion’s depth, size, or suspected pathology.
Without this explanation, payers may question whether a less costly approach could have been used. Clear documentation of technique selection significantly reduces this risk.
Diagnosis coding must align with the documented clinical concern. Non-specific or benign diagnosis codes often fail to support medical necessity for high-cost biopsies unless the documentation strongly establishes risk. When the diagnosis reflects suspicion of malignancy or uncertain behavior, the payer can more easily understand the rationale for biopsy.
Consistency between clinical notes, procedure codes, and diagnosis codes is critical for claim approval.
Many dermatology biopsy denials stem from repetitive or templated notes, missing lesion measurements, or insufficient explanation of why a biopsy was necessary at that visit. Inconsistent diagnosis coding and a lack of justification for biopsy technique selection further increase denial risk.
Addressing these issues at the documentation stage is far more effective than appealing denials after the fact.
In an audit, reviewers look for evidence of sound clinical reasoning supported by consistent documentation. When biopsy notes clearly explain lesion risk, diagnostic uncertainty, and procedure selection, they demonstrate that the service was medically necessary rather than financially motivated.
Practices that maintain this level of documentation are better positioned to withstand audits and avoid recoupments.
Arj Fatima is a medical billing and compliance content specialist at Billing MedTech. She focuses on CMS guidelines, dermatology billing accuracy, and documentation strategies that help medical practices reduce denials, stay audit-ready, and protect long-term revenue through compliant clinical documentation.
© Billing MedTech. All Rights Reserved