Are you ready to grow up your business? Contact Us
Call us anytime
Are you ready to grow up your business? Contact Us
Cardiology billing and coding is one of the most complex areas of medical billing in the U.S. It combines high-value procedures, strict documentation rules, frequent payer audits, and constant updates from CMS. Even small mistakes in coding or documentation can result in denials, underpayments, or compliance risks for cardiology practices.
This guide is written specifically for U.S. cardiologists, practice owners, and decision-makers who want a clear, practical understanding of how cardiology billing and coding work, why claims get denied, and how to protect revenue while staying compliant.
Cardiology billing and coding is the process of translating cardiovascular services into standardized medical codes and submitting them to payers for reimbursement. It involves assigning the correct CPT codes for procedures and services, linking them with accurate ICD-10 diagnosis codes, and ensuring documentation supports medical necessity.
Unlike basic office visits, cardiology services often involve diagnostic testing, imaging, interventional procedures, and long-term disease management. Because of this complexity, cardiology medical billing is closely monitored by Medicare and commercial payers.
Accurate billing is not just about getting paid. It also determines audit exposure, compliance standing, and long-term financial stability of a cardiology practice.
Cardiology services are among the highest reimbursed specialties, which also makes them a frequent target for audits. Incorrect coding, missing documentation, or improper modifier use can trigger denials or recoupments.
Accurate cardiology billing helps practices:
Improving billing accuracy directly impacts cash flow, provider productivity, and patient access to care.
Understanding the billing workflow helps identify where errors commonly occur and how to prevent them.
The billing process begins before the patient is seen. Accurate demographic information, active insurance coverage, and referral or authorization requirements must be verified. Errors at this stage often result in immediate denials.
Providers must document the patient’s condition, test results, medical decision-making, and treatment plan. Documentation should clearly justify why a cardiology service was necessary on that date of service.
Medical coders assign CPT codes for procedures and ICD-10 codes for diagnoses. These codes must align with documentation and payer guidelines before claims are submitted.
Payments, adjustments, and denials are posted to the patient account. Denied claims should be analyzed, corrected, and resubmitted promptly to avoid revenue loss.
CPT coding in cardiology includes evaluation services, diagnostic testing, and interventional procedures. Code selection must reflect the service performed, the level of complexity, and payer requirements.
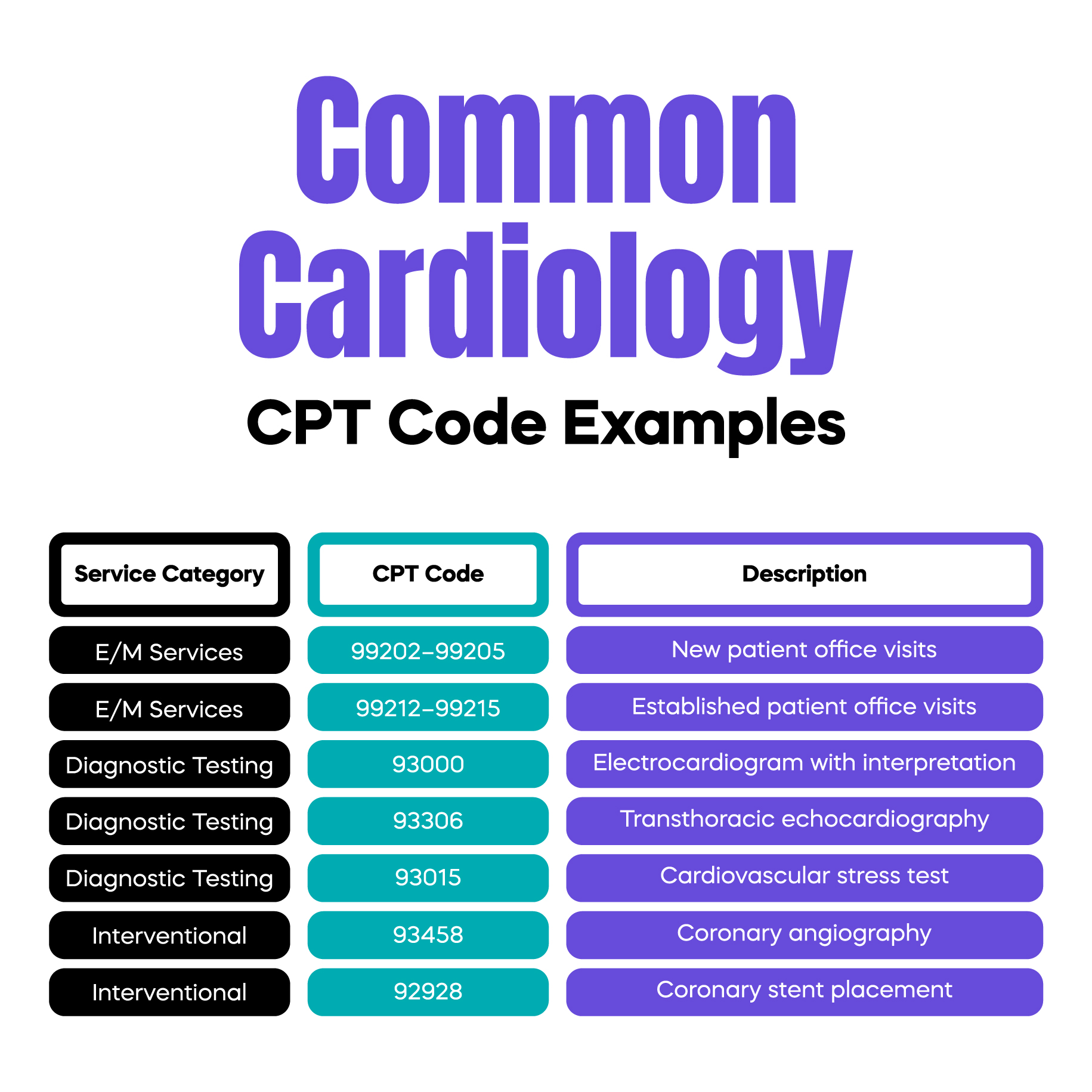
Office and hospital visit codes are commonly used for cardiology consultations and follow-ups. Accurate E/M coding depends on documentation of medical decision-making and time when applicable.
These include services such as electrocardiograms, stress tests, echocardiography, and Holter monitoring. Documentation must clearly identify whether the professional component, technical component, or both were performed.
Procedures such as cardiac catheterization, angioplasty, and stent placement require detailed procedural documentation. Small documentation gaps can lead to downcoding or denials.
ICD-10 codes explain why a cardiology service was medically necessary. Payers evaluate diagnosis codes closely to determine coverage.
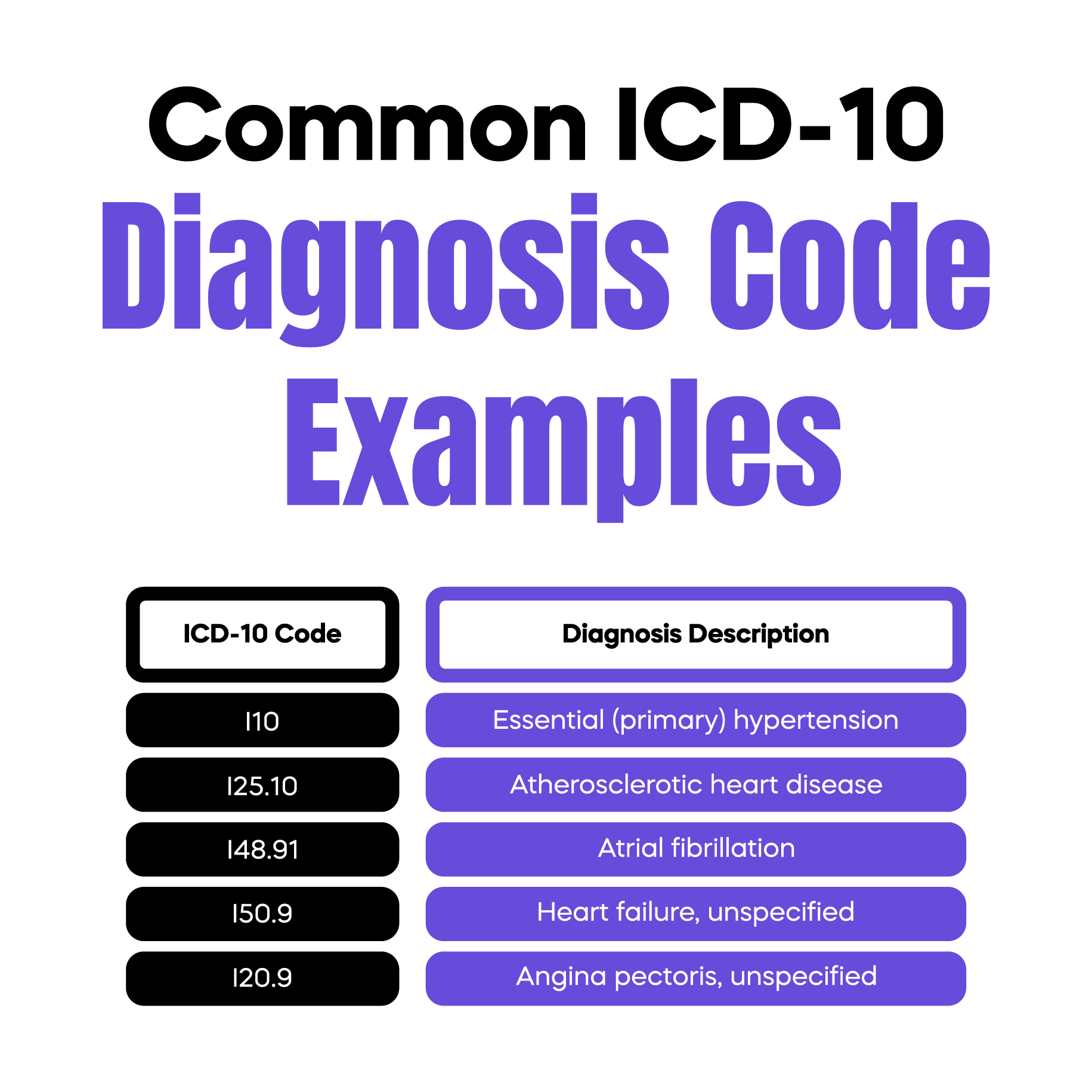
Cardiology ICD-10 codes often fall under conditions such as hypertension, ischemic heart disease, arrhythmias, heart failure, and vascular disorders.
Diagnosis codes must support the CPT code billed. If the diagnosis does not justify the service, the claim may be denied even if the procedure was performed correctly.
Documentation is the foundation of compliant cardiology billing. Every billed service must be supported by clear clinical records.
Notes should explain the patient’s symptoms, test findings, and clinical reasoning. Payers expect documentation to show why the service was reasonable and necessary.
Test results, imaging findings, and physician interpretations should be included when required. Missing reports are a common reason for denials during audits.
Modifiers communicate special circumstances that affect how services are reimbursed.
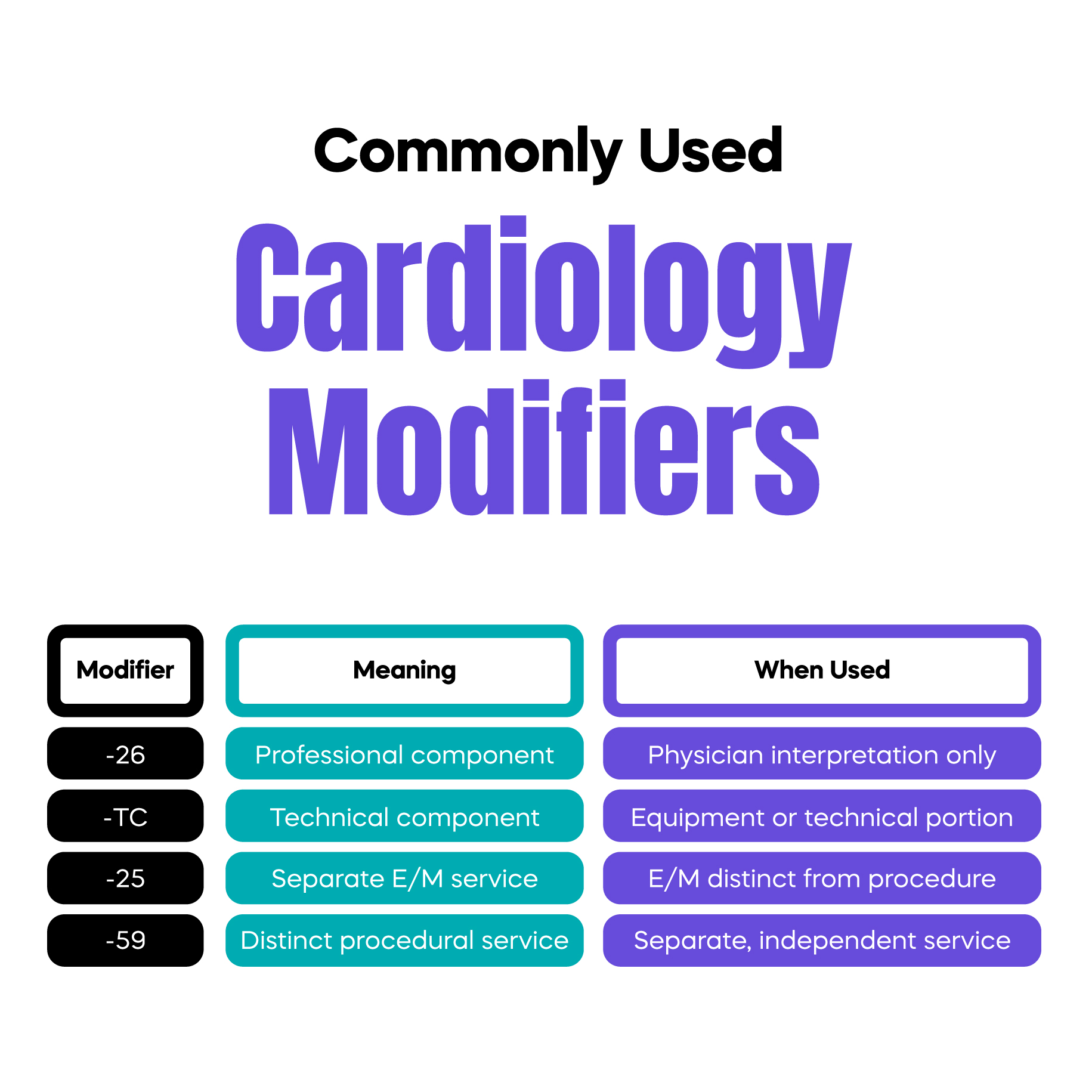
Modifiers may be required when a provider performs only the interpretation or only the technical portion of a diagnostic test.
Incorrect modifier use can trigger denials or audits. Modifiers should only be applied when documentation clearly supports their use.
Understanding denial reasons helps prevent repeat errors.
Incomplete notes or missing test reports are a leading cause of cardiology claim denials.
When CPT and ICD-10 codes do not logically align, payers may deny the claim for lack of medical necessity.
Medicare and commercial insurers often have different coverage policies for cardiology services. Ignoring these differences increases the denial risk.
Strong billing systems protect revenue and reduce administrative burden.
Accurate documentation, regular coding audits, staff education, and denial trend analysis all contribute to improved reimbursements. Practices that monitor billing performance consistently tend to experience fewer payment delays and lower denial rates.
Telecardiology and remote patient monitoring services are increasingly used in cardiology care.
Billing for these services requires the correct use of telehealth codes, time documentation, and adherence to payer-specific rules. Practices should ensure that virtual services meet coverage criteria before billing.
As cardiology practices grow, billing complexity increases. Outsourcing cardiology billing services can help practices reduce errors, stay compliant, and focus on patient care.
Professional billing teams specialize in payer rules, denial management, and revenue optimization for cardiology services.
For your convenience, we’ve prepared a printable, one-page cheat sheet summarizing commonly used CPT codes, ICD-10 codes, high-risk modifiers, documentation must-haves, and denial triggers.
You can download it here and use it as a daily reference in your practice:
Download Cheat Sheet PDF
Arj Fatima is a medical billing and coding specialist with hands-on experience in U.S. specialty billing, payer compliance, and revenue cycle optimization. She works closely with healthcare providers to improve documentation accuracy, reduce denials, and ensure compliant reimbursement.
© Billing MedTech. All Rights Reserved