Are you ready to grow up your business? Contact Us
Call us anytime
Are you ready to grow up your business? Contact Us
The QZ Modifier is one of the most scrutinized anesthesia modifiers in medical billing. For healthcare providers, especially those working with CRNAs, correct usage directly affects reimbursement, compliance, and audit exposure. While the modifier appears simple, improper application remains a leading cause of anesthesia claim denials and payer reviews.
This guide explains what the QZ Modifier represents, how Medicare and commercial payers interpret it, and how providers can bill it correctly while reducing compliance risk.
The QZ Modifier is used to indicate that anesthesia services were performed by a Certified Registered Nurse Anesthetist (CRNA) without medical direction by an anesthesiologist. From a payer perspective, QZ communicates both provider type and supervision status.
In practical terms, QZ tells Medicare and other insurers that the anesthesia service did not meet medical direction requirements. This distinction matters because supervision status directly affects payment methodology and audit scrutiny.
When QZ appears on a claim, it signals independent CRNA practice. It does not simply identify who provided care; it reflects how the anesthesia service was structured and documented. Any documentation that contradicts independent practice can place the claim at risk.
QZ is generally appropriate when a CRNA performs anesthesia services independently and medical direction requirements are not met. This often occurs in opt-out states or in practice models where anesthesiologists are not directing CRNA services. Documentation must clearly support this care model.
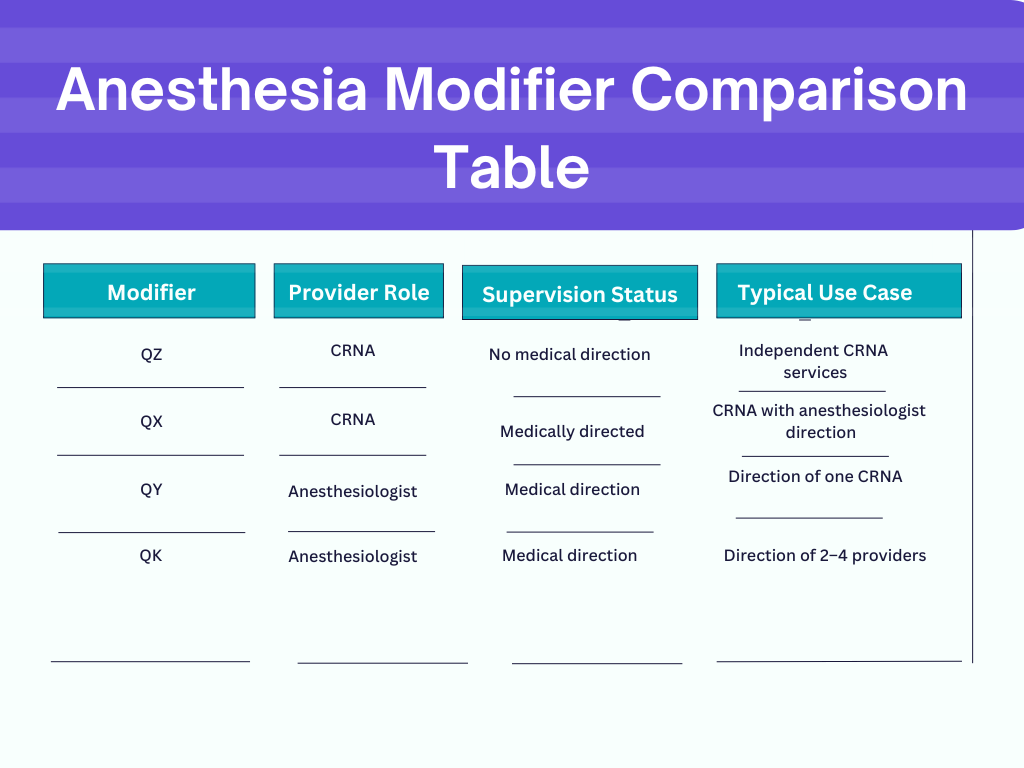
Confusion between anesthesia modifiers is one of the most common billing problems providers face. QZ is frequently misused when another modifier more accurately reflects the service provided.
The most critical distinction is between independent anesthesia services and medically directed services. QZ applies only when no medical direction exists. When any level of medical direction is present, QZ should not be reported.
Using QZ when documentation supports medical direction is a major compliance risk and frequently leads to denials or recoupments.
Medicare allows the QZ Modifier when anesthesia services are performed by a CRNA without medical direction. CMS focuses heavily on documentation consistency. Even in opt-out states, Medicare expects records to reflect the actual supervision model used.
In opt-out states, physician supervision is not required under Medicare. However, opt-out status does not eliminate the need for accurate documentation. If the record suggests physician involvement, billing QZ may be inappropriate.
QZ claims are reimbursed differently than medically directed services. Incorrect modifier usage can result in payment adjustments or post-payment review, particularly for high-volume anesthesia providers.
Accurate billing starts with aligning documentation, supervision status, and modifier selection.
The QZ Modifier is used with anesthesia CPT codes and should be placed correctly on the claim according to payer rules. Incorrect sequencing or incompatible CPT combinations often result in rejected claims.
Documentation should clearly demonstrate independent CRNA involvement. Records should avoid language that implies anesthesiologist direction or supervision. Inconsistencies between clinical notes and billing modifiers are a frequent source of denials.
CRNAs billing with QZ must practice within state scope-of-practice rules and payer policy guidelines. Credentials, licensure, and documentation must all support independent practice.
Many QZ denials stem from anesthesia records that include physician signatures, supervision language, or unclear provider roles. These details can contradict the intent of the modifier and trigger payer review.
Denials often occur when claims include conflicting modifiers, incomplete anesthesia records, or documentation that suggests medical direction. Commercial payers may also apply stricter interpretation than Medicare.
Correcting denied QZ claims requires a careful review of documentation and billing alignment. Preventive strategies include regular modifier audits and standardized anesthesia documentation practices.
QZ claims are frequently reviewed because they directly impact reimbursement structure. A high percentage of QZ usage or inconsistent modifier patterns can draw payer attention.
Providers can reduce audit risk by conducting internal reviews, maintaining consistent documentation language, and ensuring billing reflects actual care delivery models.
Written by a U.S. medical billing compliance specialist with more than 10 years of experience in anesthesia billing, CRNA reimbursement, Medicare policy interpretation, and audit defense for physician practices and hospitals.
© Billing MedTech. All Rights Reserved